College of Medicine and Public Health
Transforming Health, Inspiring Futures
At Flinders University, the College of Medicine and Public Health is dedicated to improving health outcomes through world-class education, impactful research, and workforce development. Our integrated approach, spanning clinical training, population health, and laboratory science, supports the health and wellbeing of individuals and communities across Australia.
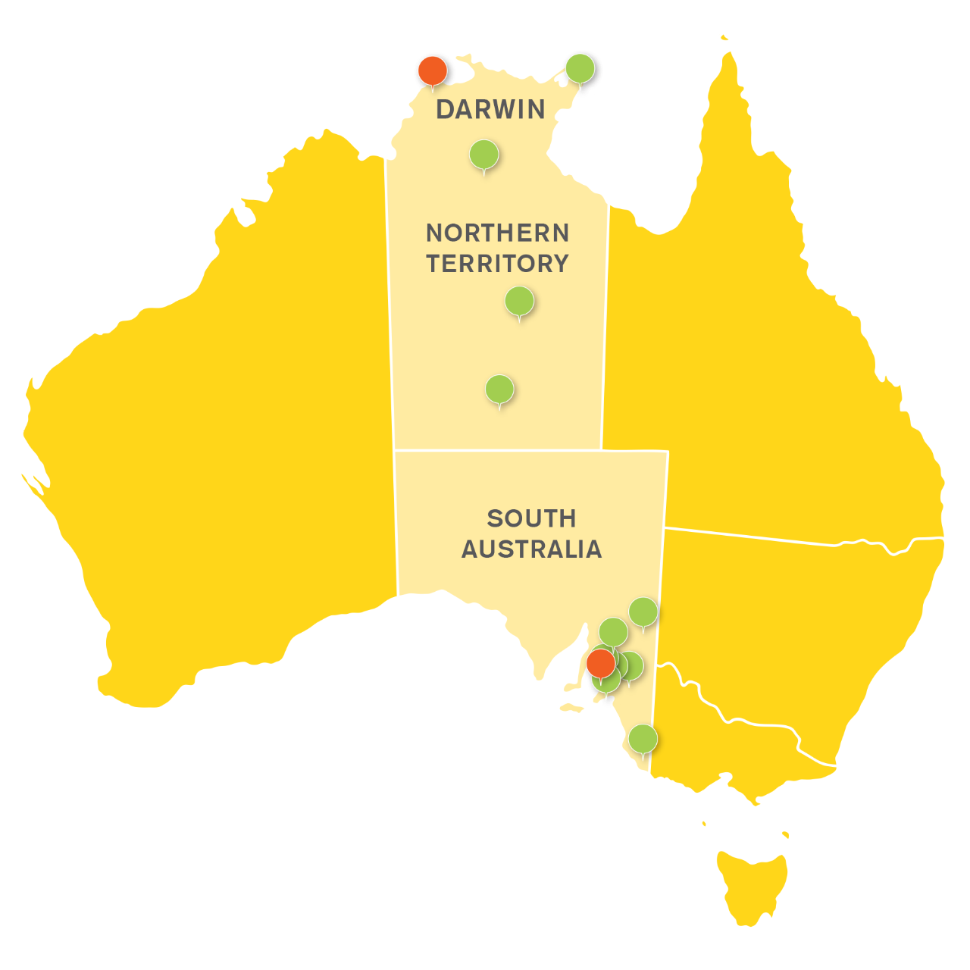
With a distinctive footprint stretching from metropolitan Adelaide through rural South Australia to remote communities in the Northern Territory, we are deeply embedded in the regions we serve. This unique reach underpins our strong commitment to health equity and ensures that our programs, research, and partnerships reflect the needs and priorities of diverse populations.
At the heart of the College, the Flinders Health and Medical Research Institute (FHMRI) is leading life-changing research that connects molecular discovery with community-led health initiatives. FHMRI addresses the most pressing health challenges by advancing precision medicine, innovating clinical care, strengthening health systems, and driving public and population health outcomes.
Our strategic research priorities are reflected in our Flagship Programs—Sleep Health and Eye and Vision—as well as Impact Programs in Health Equity and Cancer. These initiatives embody our focus on real-world impact and evidence-based solutions.
FHMRI's bold vision to eliminate disease and reduce health inequities is powered by cutting-edge investigations and collaborative partnerships. Researchers work closely with health practitioners, patients, and global networks, supported by state-of-the-art facilities and a culture of innovation, inclusion, and excellence.
We are proud to lead nationally in Indigenous and Rural and Remote Health research, partnering with communities to close the gap and improve outcomes where the need is greatest.
Through our commitment to education, the College is shaping the next generation of doctors, clinicians, and health professionals. Our graduates are equipped with the knowledge, skills, and compassion to build a healthier, fairer future.
At the College of Medicine and Public Health, our work doesn't just generate knowledge—it transforms lives.
Rural and Remote Health SA & NT
Flinders University has a geographic footprint throughout the Central Australian Corridor.
The College of Medicine and Public Health’s collective vision is to be recognised as the global leader in producing a committed, highly skilled and culturally safe rural and remote health workforce, and rural and remote health research; both of which pay attention to the needs of our First Nations communities.

Scholarships
The College of Medicine and Public Health have a variety of scholarships available to students to help with their education.
Eligibility and scholarship criteria apply, please see within each scholarship opportunity listed for more information.
Higher Degree by Research - Industry Engagement
Do you share our passion for discovery?
Solve complex problems and explore new ways of doing things through a PhD Industry Partnership.
![]()
Sturt Rd, Bedford Park
South Australia 5042
South Australia | Northern Territory
Global | Online
CRICOS Provider: 00114A TEQSA Provider ID: PRV12097 TEQSA category: Australian University