Sleep FAQs
Sleep, exercise and healthy eating are the corner stones of leading a healthy life. Missing out on sleep or having a sleep disorder that robs you of good quality sleep can have serious short- and long-term health consequences.
Poor sleep can result in memory and mood disturbance and lead to daytime sleepiness, poor concentration and accidents. In the long-term, chronic sleep deprivation may contribute to a host of health problems including obesity, diabetes and cardiovascular disease. Sleep disorders are varied and can affect anyone at any time.
If you are seeking more information about sleep health and disorders, we have useful information available for:
Common sleep issues
Obstructive sleep apnea
Obstructive sleep apnea (OSA) is a common disorder of sleep affecting twice as many men as women. It usually occurs in mid-life, but can affect people at any age. People with OSA experience repeated collapse of their upper airway while asleep, resulting in poor sleep quality and, in some cases, low blood oxygen levels.
Common features
- Obesity (a major risk factor)
- Long-standing snoring
- Stop breathing episodes in sleep, as noticed by the bed partner
- Morning headache and/or dry mouth
- Excessive sleepiness during the day, sometimes including an increased risk of fall-asleep motor vehicle accidents
- Untreated severe OSA may increase the risk of developing high blood pressure, diabetes, stroke and heart disease
Diagnosis
Diagnosis usually involves an overnight sleep study in a hospital. This commonly performed procedure enables doctors to measure your breathing and sleep patterns, as well as your blood oxygen levels while you are asleep, and thus determine the presence and severity of OSA.
Treatment
There are several treatments for OSA. Most patients use a device called continuous positive airway pressure (or, more commonly, CPAP), which is a pump that uses air pressure to splint open the airway at night. In milder cases, avoiding sleeping on your back or a dental splint can be helpful. Weight loss is an important part of the treatment in many, if not most, patients. Surgery for the upper airway is also an option for selected patients.
Central sleep apnea
Central sleep apnea (CSA) is a disorder in which a person's breathing repeatedly stops and starts during sleep because the brain temporarily stops sending signals to muscles that control breathing. Unlike obstructive sleep apnoea there is no obstruction or blockage of the upper airway.
Diagnosis
Diagnosis of CSA involves an overnight sleep study to detect and measure the severity of the condition.
Treatment
There are several potential treatments for CSA including continuous positive airway pressure (CPAP), bi-level positive airway pressure, adaptive servo-ventilation, oxygen therapy, and certain types of medications.
People with central sleep apnoea will be advised by a sleep specialist as to the type of treatment they need following a sleep study.
Restless legs syndrome (RLS) and periodic leg movements in sleep (PLMS) are relatively common conditions that usually affect older adults. RLS and PLMS commonly occur together and are generally treated in the same manner. They may be associated with underlying medical conditions, such as diabetes or kidney diseases. A number of different treatments are available which have been shown to be effective in both RLS and PLMS.
Restless legs syndrome
RLS is usually described as creeping sensations in the legs, accompanied by a strong desire to move the legs. These symptoms are worse at rest. They usually occur in the evening and may get worse as the evening progresses. As a result, patients with RLS may have difficulty falling asleep.
RLS affects approximately 5-15% of the population. This chronic movement disorder may begin at any age, but the symptoms typically become more pronounced in the above 40 age group. In fact, symptoms tend to become worse and more frequent as the sufferer grows older.
More females are affected than males, and females tend to report more symptoms as well. Although the name suggests a leg movement disorder, the restlessness and discomfort may spread to involve the arms in about 20-30% of more severely affected patients. One in five patients may report the abnormal sensations to be painful.
About 80% of patients with RLS also experience PLM in sleep.
Periodic leg movements in sleep
PLMS consists of frequent rhythmic movements of the legs and feet during sleep. People with PLMS are often described as restless sleepers and they may feel tired during the day due to the sleep disruption caused by the leg movements in sleep. PLMS is easily diagnosed by an overnight stay in hospital for a sleep study.
PLMS is a term used to describe a series of complex, involuntary, repetitive and stereotypic upward movements involving upward motion of the big toe, downward and fanning motion of the other toes and accompanied by bending of the ankle, knees and thighs. PLMS is measured in the sleep laboratory using electrodes placed on the skin on the front of the legs (anterior tibialis muscles). Leg movements are scored as PLMS if occurring in a sequence of four or more movements lasting 0.5 to 5 seconds each episode and recurring every 20-40 seconds.
Do you have restless legs syndrome?
If you frequently experience the following symptoms, you may have RLS with or without accompanying PLMS.
- An irresistible urge to move the legs, usually accompanied or caused by unpleasant sensations in the legs such as tingling, crawling, creeping, cramping, burning or even pain.
- Beginning or worsening of these symptoms when resting or inactive such as when sitting down to watch television, travelling in a car or aeroplane, or lying down to sleep at night.
- A partial or total relief with movement (such as stretching or getting out of bed to walk), rubbing of the legs, or having a bath.
- Worsening of the symptoms in the evening or at night.
- Involuntarily kicking or twitching of the legs in sleep.
If you do have RLS, you are not alone. Approximately five out of every 100 people will experience RLS at some point in their life.
Who needs treatment?
This depends on the severity and frequency of the symptoms. In all patients, associated factors should be treated or removed where possible as this may decrease or abolish symptoms of RLS.
Mild or infrequent symptoms
Medications are generally not required in mild cases. Simple remedies such as the following may be adequate:
- Decrease caffeine, avoid alcohol and nicotine.
- Exercises focusing on stretching or bending (e.g. yoga).
- Hot or cold packs to affected limbs.
- Hot or cold baths.
- Massage or rubbing of limbs.
- Mental alerting activities (e.g. crossword puzzles).
In those with reduced iron stores, iron supplementation may be considered after exclusion of potential causes (e.g. bleeding, dietary deficiency, kidney failure). Concurrent supplementation with vitamin C to aid iron absorption may be helpful.
Severe or frequent symptoms
The most common medications for RLS and PLM are:
- Dopaminergic agents, which increase the level of dopamine in the brain. These are the medications of choice for treatment of RLS and PLM and are taken an hour or two before bed.
- Dopamine precursors were the earliest medications used; examples are Sinemet and Madopar. These medications can be quite effective. However, because they are short-acting, a phenomenon called 'augmentation' occurs commonly (65-80% of cases). Augmentation typically occurs several months after starting treatment and is characterised by symptoms appearing earlier and earlier in the day, and often intensifying in severity. Higher doses of these medications typically worsen rather than resolve augmentation.
- Dopamine agonists are newer medications that do not commonly cause augmentation. Earlier agents such as cabergoline contained a substance called 'ergot.' Because of rare reports of thickening of the heart valves and lining of the lungs ergot-containing medications are no longer recommended for RLS . Newer medications such as ropinirole and pramipexole do not contain ergot and are now preferred. Doses are commenced low and increased gradually to reach a steady level, tailored to the individual patient’s response. Side effects such as nausea and headaches are usually mild and transient.
- Benzodiazepines have a relaxing effect and slow down the central nervous system. They promote sleep and reduce RLS symptoms. Clonazepam is the most commonly used benzodiazepine for RLS. Its success in treating RLS is limited by its likelihood to cause side effects (next-day drowsiness) and reduced efficacy (tolerance) in long-term use.
- Opioids are pain-killing, relaxing medications. Similar to the benzodiazepines, the potential for abuse is low when used in patients with RLS. Codeine is the most common opioid used for RLS. Aperients may be needed for those that develop constipation with opioids.
- Anticonvulsants may be effective especially in patients who experience painful sensations with RLS. Gabapentin is most commonly used for these patients. Potential side effects are next-day drowsiness and unsteadiness, particularly in higher doses. As gabapentin may cause a rare, but potentially serious, blood reaction, some blood tests are performed in the course of using this drug.
Can restless legs syndrome or periodic leg movements affect my sleep?
People with RLS may complain of varying degree of leg discomfort during the daytime. Some people may even experience problems with memory and concentration. However, many people are affected most significantly at bedtime as the symptoms are worse with inactivity and at night, and this makes it difficult to fall asleep. It is not uncommon for them to get up several times to walk around until symptoms are partially relieved.
On the other hand, PLMS occurs when the person is already asleep and can range in intensity from mild twitches to violent kicks. Although the peak of PLMS activity typically occurs in the early part of sleep, leg movements may be present for the entire night in more affected individuals. In the laboratory, PLMS is considered severe if it occurs 50 times or more per hour—especially if movement causes frequent brief awakenings (arousals) at least 25 times per hour. Generally, people with PLMS are not consciously aware of these awakenings, but if they occur very frequently, sleep may be severely disrupted resulting in excessive daytime sleepiness. PLMS may also result in the bed partner being kicked, sometimes violently, and wearing out of bedsheets on some occasions.
Can RLS/PLM cause sleep apnea?
The answer is no, although the two conditions may interact.
- Obstructive sleep apnea (OSA) is a condition where patients stop breathing very frequently during sleep, sometimes hundreds of times each night. Patients with OSA may sometimes have leg jerks during the night as a consequence of the upper airway repeatedly closing and opening. These leg jerks will disappear when the patient’s OSA is treated with continuous positive airway pressure (CPAP).
- Conversely, PLM, particularly if severe, can disrupt sleep and worsen mild OSA. Successful treatment of PLM can result in an improvement in OSA in such a case.
A sleep study can therefore be of value in certain patients, if another cause of sleep disturbance such as OSA is suspected, and needs to be confirmed.
Insomnia is common and affects people of all ages. There are many different reasons for insomnia. Conditioned sleep-related behaviours or habitual insomnia are the most common causes. Less commonly, insomnia may be due to side effects of certain medications or an underlying medical disorder such as depression.
Common features
- Difficulty getting off to sleep
- Trouble staying asleep
- Waking too early in the morning
- Worrying about not sleeping
- Tiredness during the day
How to improve your sleep related behaviours
- Avoid alcohol and caffeine-containing drinks after 6pm
- Use the bedroom for sleeping and intimate activity only (e.g. not for studying, working or watching television)
- Avoid long daytime naps
- Aim to rise at the same time each day
- Avoid excessive time in bed
- If unable to sleep, stay out of bed until sleepy again
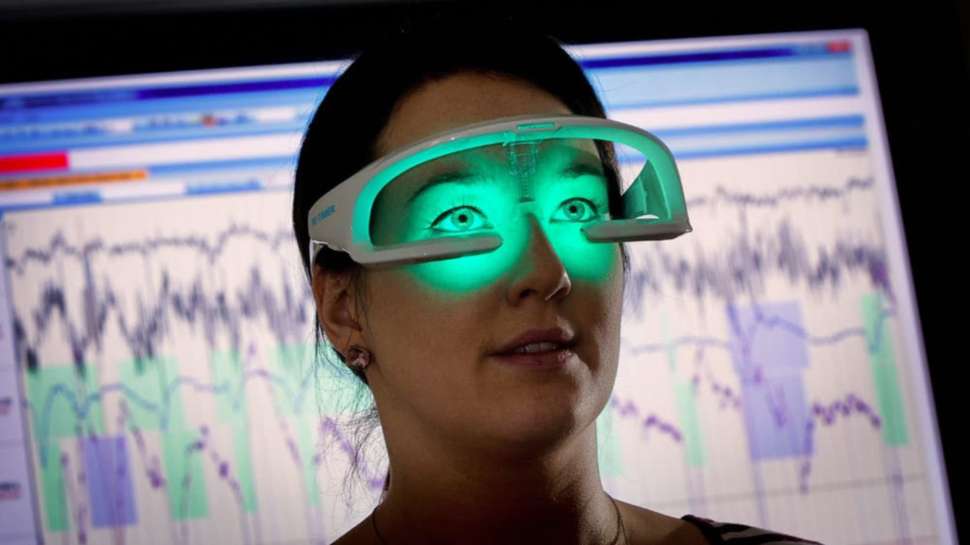
Other strategies to treat conditioned insomnia include relaxation techniques and more specialised methods such as Stimulus Control and Sleep Restriction Therapies. Some types of insomnia may be caused by a mistimed body clock, which can be treated with bright light therapy. You may have seen the light therapy devices to treat certain types of insomnia related to body clock mis-timing on the SBS program, "Australia's Sleep Revolution". Enquiries about them can be directed to: re-timer.com
Narcolepsy is a neurological disorder in which the brain is unable to regulate the sleep-wake cycle normally. It is a chronic disorder that affects approximately 0.05% of the population. This translates to roughly one in every 2000 people. While the cause of narcolepsy is not fully understood yet, scientists have found genes associated with this disorder. The likelihood of developing narcolepsy is increased if an individual has a particular type of genetic makeup, termed HLADQB1*0602.
Symptoms
- Excessive sleepiness during waking hours for no apparent reason. This is usually the first symptom to appear.
- Falling asleep in inappropriate situations such as when talking to someone, working or driving.
- Feeling weak or sudden collapse during periods of strong emotions (e.g. laughter, anger, fear).
- Vivid nightmares immediately before falling asleep or waking up.
- Paralysed immediately before falling asleep or waking up.
Treatments
There is currently no treatment that can reverse narcolepsy. Treatment with medications is the first line of defence against debilitating symptoms. However, changes in behaviour are equally important and when combined with drug treatment have helped most people with narcolepsy improve their alertness and enjoy an active lifestyle.
A woman with narcolepsy who is pregnant (or is thinking about becoming pregnant) should speak to her physician about the possible effects of her medication on the child.
Narcolepsy and driving
A common misconception of people with narcolepsy is that they should not drive. The good news is that diagnosed and medically treated patients with narcolepsy appear no more at risk for road accidents than the general public.
Parasomnias are abnormal movements or behaviours in sleep. Different types include:
Sleepwalking and night terrors
These are relatively common in children and young adults and will normally get better with age. In severe cases—such as those which cause significant sleep disruption or risk of injury—further investigation and treatment may be needed. Sleepwalking and night terrors are less common in adults and if present, will often require investigations to exclude other medical disorders.
REM Behaviour Disorder
REM behaviour disorder is a fascinating disorder from both a neurological and sleep point of view. People usually have dreams during rapid eye movement (REM) sleep. There is normally a profound paralysis of the body's muscles during REM sleep; however, people with parasomnias do not experience paralysis in this stage of sleep. Thus patients often act out their dreams, particularly if violent.
Symptoms
Parasomnias usually manifest as repetitive violent movements during REM or 'dreaming sleep,' which can sometimes result in injury to both the patient and their bed partner. Patients are often aware that they have been dreaming during these episodes.
Parasomnias usually occur later in life. Some patients may later develop Parkinson's disease.
Diagnosis and treatment
It is important to exclude other sleep disorders that may appear similar to this condition by having a sleep study. Treatment with certain medications is usually extremely effective.
A number of medical conditions may be associated with disorders of sleep. In some cases, severe obesity alone may also lead to breathing abnormalities in sleep.
Patients who develop sleep-related breathing problems may commonly experience morning headaches, daytime sleepiness or difficulty concentrating during the day. It is vital to recognise these problems when they exist, as they may lead to worsening of the underlying condition. For conditions associated with breathing abnormalities in sleep treatment similar to that for obstructive sleep apnea (OSA) is often effective.
A few examples of other conditions associated with sleeping disorders are:
- Hypertension (high blood pressure)
- Heart failure
- Parkinson's disease
- Chronic pain syndromes treated with opiate medications
- Muscular dystrophies including Motor Neurone Disease
Obesity hypoventilation syndrome
Some cases of severe obesity may lead to persistent underbreathing or 'hypoventilation' during sleep. People who develop obesity hypoventilation syndrome commonly experience night-time or morning headache, daytime sleepiness or difficulty concentrating during the day. They may develop progressive respiratory failure in the daytime as well.
Hypertension / High blood pressure
This disorder is frequently associated with obstructive sleep apnea, particularly in people with difficult to control blood pressure (i.e. needing three or more blood pressure medications). In short term studies, treatment of obstructive sleep apnoea has been shown to improve blood pressure control. If someone with high blood pressure has symptoms to suggest sleep apnoea it is important to check for this condition.
Heart failure
Heart failure is strongly associated with both obstructive sleep apnoea and a condition called central sleep apnea or Cheyne Stokes Respiration. In central sleep apnoea, subjects recurrently stop breathing. This is the result of abnormal control of breathing, not airway obstruction. More than 40% of people with heart failure have either obstructive sleep apnoea or central sleep apnoea or both. Treatment of obstructive sleep apnoea has been shown to improve the function of the heart in short term studies. While treatment of central sleep apnoea may improve symptoms of sleep disruption, it has not yet been shown to improve heart function.
Parkinson's disease
Parkinson's disease is often associated with excessive daytime sleepiness. This may be due to the sleep disruption caused by stiffness and abnormal movements or the disease process itself. Some of the medications used to treat Parkinson's disease have been associated with—what have been described as—sleep attacks.
Chronic pain syndromes treated with opiate medications
Having a chronic pain disorder, not surprisingly, may interfere with sleep quality. It is becoming apparent, however, that being on high doses of opiate pain medications may predispose to abnormal breathing at night—which is a form of central sleep apnoea syndrome. This may contribute to additional sleep disruption and can be difficult to treat medically. Reducing the dose of opiates to the minimum required to maintain pain control may help.
Muscular dystrophies including Motor Neurone Disease
The muscle weakness caused by chronic pain disorders may cause significant underbreathing at night. This causes the waste gas carbon dioxide to build up at night and a low oxygen level during sleep. Symptoms of sleep-related breathing abnormality in neuromuscular conditions like motor neurone disease may include shortness of breath while lying flat, gasping at night and morning headaches. These symptoms can be eased considerably by a machine to assist breathing at night.
Useful websites for further information
Australasian Sleep Association
A peak scientific body in Australia and New Zealand representing clinicians, scientists and researchers working in sleep health and sleep medicine. Both provide education and training to members and the broader health community in Australia and New Zealand.
Australia's Leading Consumer Advocate for Healthy Sleep provides a range of resources for the public.
Secondary school students FAQs
The researchers at FHMRI Sleep receive many requests to provide information or interviews to assist with senior high school research projects. To assist with these queries, we have put the following additional information together to help in your research about sleep. If you have any further queries, please contact us.
Contact us
Get in touch to chat to us about our research or community engagement opportunities.
Find us at:
Adelaide Institute for Sleep Health
Level 2, Building A
Mark Oliphant building
5 Laffer Drive
Bedford Park 5042 SA

![]()
Sturt Rd, Bedford Park
South Australia 5042
South Australia | Northern Territory
Global | Online
CRICOS Provider: 00114A TEQSA Provider ID: PRV12097 TEQSA category: Australian University